Endovascular robotic systems: Toward new therapeutic horizons
- Ameco

- Jun 14, 2021
- 6 min read
Updated: Aug 20, 2021
When robotic systems provide higher precision, better access, standardization and improved outcomes, what will the future of endovascular interventions look like?

Imagine a time when every stroke patient has immediate access to minimally-invasive treatment. When every cardiac stent is placed as precisely as possible. When young doctors collaborate remotely with experienced colleagues across institutions. Welcome to the robotic future of endovascular interventions.
Interventional therapies both in cardiology and in neuroradiology are among the most fascinating innovations in modern healthcare. Hundreds of thousands of patients with myocardial infarction or chronic coronary artery disease are treated with percutaneous coronary interventions (PCI) each year. Neurosurgical procedures are increasingly being replaced by less invasive endovascular therapies. And with mechanical thrombectomy, a completely new minimally-invasive approach to stroke care is currently being rolled out in countries all over the world. In this type of intervention, neuroradiologists “unblock” cerebral arteries by removing blood clots with a catheter-based intervention, which, if successful, improves stroke outcome substantially.
How to address access and quality issues?
Interventional therapies offer huge benefits over open surgical approaches in treating a variety of diseases. But there remain some challenges: “When we look at neuroradiology, this is a highly specialized subspeciality in medicine. Training takes years, experienced experts are scarce, and access to treatment is far from universal”, says Pasquale Mordasini, MD, experienced neurointerventionalist at the University Institute of Diagnostic and Interventional Neuroradiology at Inselspital Bern in Switzerland. In cardiology, which is one or two decades ahead of neuroradiology in embracing endovascular interventions on a broad scale, the situation is somewhat different. At least in the industrialized world, cardiac catherization is widely available. But not every institution achieves the same standards, according to J. Aaron Grantham, MD, cardiologist at St. Luke’s Mid America Heart Institute and Chief Medical Officer at Corindus:
“To me, the biggest challenge in interventional cardiology is the variability in care. Patients don’t have access to the same level of care everywhere. This is a very big problem that needs to be addressed.”
Gaining precision in cardiac interventions
Can it be addressed? Enter robots. With cardiologists in the driver’s seat, the introduction of robotics is increasingly gaining momentum in interventional medicine – and there is huge potential for both better access to care and better patient outcomes. Endovascular robotics is not about some machine performing surgery on its own. It is about robotic systems operated and closely monitored by specialists in the field, geared towards reducing errors, increasing quality, and improving access. In cardiology the future is already here: robots are increasing precision and helping to achieve better outcomes. The main area is percutaneous coronary interventions (PCI) , where cardiologists have to decide when to use a stent and how to place it as precisely as possible. Endovascular robotic solutions can help with this, says Grantham, and he gives an example: “There is a problem called longitudinal geographic miss, which is a situation in which a stent doesn’t cover the entire length of a stenosis. We have shown that we can substantially reduce longitudinal geographic miss with a robotic system. And we have also demonstrated an overall reduction in stent use.” Longitudinal geographic miss refers to the fact that a stent may not always be ideally placed if the cardiologist relies purely on a visual estimate. A robot, in contrast, can measure the anatomy exactly and place the stent with a precision of 1mm, which will improve PCI outcome for the patient.

Improving access to state-of-the-art stroke care
Precision is, of course, an issue in neurovascular interventions, too. But here it is access to care that is the real challenge. This is especially true for mechanical thrombectomy, a highly successful yet fairly recent interventional therapy for patients with ischemic stroke . Even in highly industrialized countries, only a fraction of stroke patients eligible for interventional therapy actually receive it. And in many less industrialized countries, the therapy isn’t even available.
There are several reasons for this. The infrastructural requirements of institutions planning to offer interventional stroke care greatly exceed those in cardiology. More importantly, there are simply not enough neuroradiologists capable of performing these complex interventions. And this is where Mordasini sees endovascular robotics come into play in the coming years: “I think one of the most obvious scenarios is that we might be able to create hub-and-spoke networks with interventional robots in spoke hospitals and highly experienced neuroradiologists in the expert hub. This would allow us to increase access to interventional stroke care substantially, and also to enhance quality and ultimately improve outcomes.”
From on-site thrombectomy to tele-coaching and remote interventions
According to Mordasini, there are several possible scenarios regarding how such interventional stroke care networks could be organized in an age of endovascular robotics. One is a scenario in which neuroradiologists from the specialized institutions use robotic systems in the spoke hospitals to perform truly remote procedures. This could be an attractive choice for regions that lack neuroradiological expertise altogether. Another scenario is a “coaching” scenario in which less experienced interventional experts on-site perform the mechanical thrombectomy with a robotic system, assisted, if necessary, by experienced experts in thrombectomy who act as a backup in situations that turn out to be more complex than expected. Apart from improving access to interventional stroke care, this kind of scenario, says Mordasini, could also be very helpful in the training of younger colleagues: “It is like learning to drive a car with a driving teacher: They don’t drive themselves, but they are always there to help if necessary.”
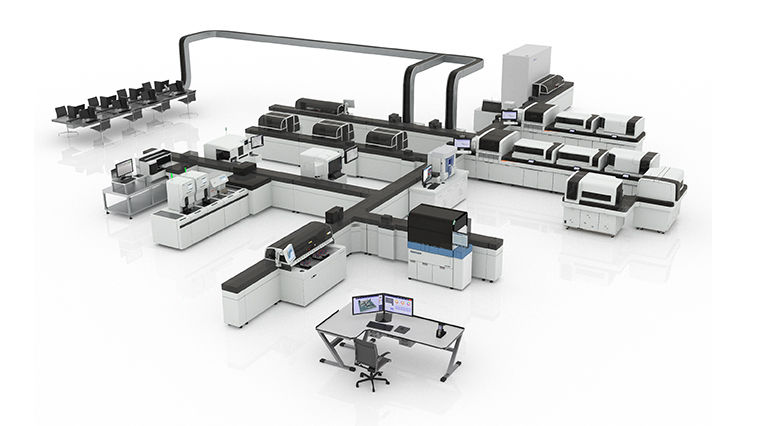
The interventional lab will look different…
With or without coaching or remote interventions, there is little doubt that the interventional lab or hybrid OR will look different in a robotic future. This can already be seen in cardiology: “The way we install robotic systems now is that we no longer put the cockpit in the examination room. The screen and the console are placed in the control room behind leaded glass. So the cardiologist is already separated from the patient at least part of the time.” This has multiple advantages, the most obvious during a pandemic being that it allows the interventional cardiologist to keep a distance from a possibly infected patient: “It might be too late for this pandemic, but there is certainly an opportunity here to protect people in the future, especially the operator,” says Grantham. “There is a group in Brazil doing research on this topic. They are measuring how much time staff spend within and beyond six feet of the patient, but ultimately, they will have to prove that robotic systems prevent infections, which is a bit harder to do.”

… and radiation exposure will be reduced
Apart from infections, another safety aspect is radiation exposure. This is an issue both in cardiology and in neuroradiology – for the patients, but even more so for the staff, as Mordasini explains: “In neuroradiology, we have interventions that may take three, four, five or even six hours, and many of us are doing this for our whole professional life. Robotic systems have a huge potential to reduce staff radiation exposure.” There is, in fact, already some data available in cardiology. In coronary artery disease patients with a chronic total occlusion (CTO), the blood vessel is totally blocked, usually over a distance of several centimetres, and the therapeutic goal is to reopen it: “The first step in these patients is crossing the occlusion with an over-the-wire microcatheter, which at the moment cannot be done robotically. So, what I usually do is I cross the occlusion manually, then switch to a rapid-exchange gear and do the rest of the procedure robotically”, explains Grantham. This “semi-robotic” approach has a radiation exposure dimension: “We published a retrospective analysis of 75 CTO procedures with the University of Washington and showed that the operator spends 48 per cent of the procedure time with the robot . We are now conducting a randomized controlled trial in which we actually measure radiation exposure with dosimeters so that we can directly compare a fully manual CTO procedure with a robotically-assisted procedure. I have little doubt that we will be able to prove a marked reduction in staff radiation exposure.”
New therapeutic options ahead?
But potentially the most exciting thing about robotic systems in endovascular care is that they could evolve into something much bigger, especially in neurovascular procedures, according to Mordasini:
"Mechanical thrombectomy in stroke will come first, but I think that over time, we will have many more interventions that will be suitable for robotics. This is because we really have to work very precisely. We are navigating in delicate and complex anatomical structures. I really think that neuro-interventions can develop from robotics and become an even more powerful tool."
Pasquale Mordasini, MD, Neurointerventionalist, University Institute of Diagnostic and Interventional Neuroradiology, Inselspital Bern, Switzerland.




Comments